Hemorrhoidectomy: Surgical Treatment for Hemorrhoids
Understanding the Purpose and Procedure of Hemorrhoidectomy
Hemorrhoidectomy is a surgical procedure performed to treat severe cases of hemorrhoids. Hemorrhoids, also known as piles, are swollen and inflamed blood vessels in the rectum or anus that can cause discomfort, pain, and bleeding. When conservative treatments such as lifestyle changes, medications, and non-surgical interventions fail to provide relief, a hemorrhoidectomy may be recommended.
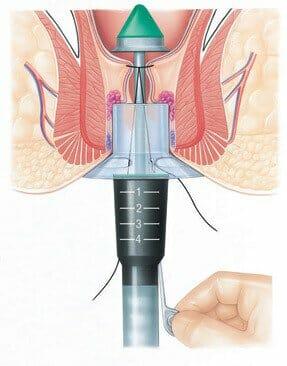
During a hemorrhoidectomy, the patient is placed under general anesthesia or regional anesthesia. The surgeon removes the hemorrhoidal tissue, which can be internal, external, or both. The procedure can be performed using various techniques, including conventional excisional hemorrhoidectomy or newer methods like stapled hemorrhoidopexy or laser hemorrhoidectomy. The choice of technique depends on the specific case and the surgeon's expertise.
Recovery and Post-Operative Care
Following a hemorrhoidectomy, patients typically require a period of recovery. It is common to experience pain, swelling, and discomfort in the surgical area, which can be managed with pain medications prescribed by the doctor. Stool softeners and dietary modifications, such as consuming fiber-rich foods and drinking plenty of fluids, may also be advised to prevent constipation and strain during bowel movements.
It is important to maintain proper hygiene to avoid infection. Patients are advised to take warm baths (sitz baths) and gently clean the area after each bowel movement. The surgeon will provide specific instructions on wound care and when to resume normal activities, including work and exercise.
Potential Risks and Complications
Like any surgical procedure, hemorrhoidectomy carries potential risks and complications. These may include:
Bleeding: Mild bleeding during bowel movements is normal after surgery, but excessive bleeding may require medical attention.
Infection: Although rare, infections can occur at the surgical site. Signs of infection include increased pain, redness, warmth, or discharge from the incision site.
Pain and discomfort: It is common to experience pain and discomfort in the rectal area after surgery. This can be managed with pain medications and the recommended post-operative care.
Anal stenosis: In some cases, the surgical site may heal with scarring, leading to narrowing of the anal canal (anal stenosis). This can cause difficulty in passing stools.
Fecal incontinence: Rarely, patients may experience difficulty controlling bowel movements (fecal incontinence) following surgery. This is more common in cases involving extensive removal of tissue. It is essential to follow the surgeon's instructions and attend follow-up appointments to ensure proper healing and address any concerns or complications that may arise.
In conclusion, hemorrhoidectomy is a surgical treatment option for severe hemorrhoids that do not respond to conservative measures. The procedure involves the removal of hemorrhoidal tissue and can provide long-lasting relief. While there are potential risks and complications associated with the surgery, most patients experience successful outcomes and improved quality of life after undergoing hemorrhoidectomy.
We are associated with experienced and highly skilled medical professionals. We use the latest medical technology available in the world and we provide medical services in collaboration with JCI & NABH Certified hospitals only. Our services include various types of treatment and organ restructuring and transplant.
