Cloacal Malformation Surgery: Treatment and Procedures | Medical Insights
Understanding Cloacal Malformation
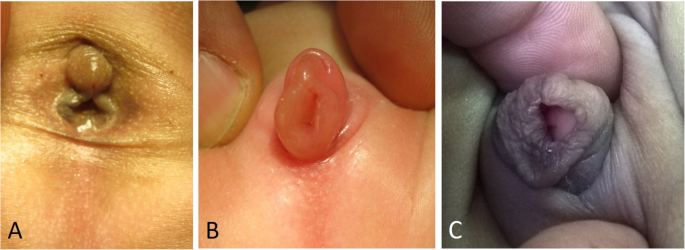
Cloacal malformation is a rare congenital anomaly that affects the development of the urinary, digestive, and reproductive systems in infants. Normally, during fetal development, separate structures form for the bladder, rectum, and genitals. However, in cases of cloacal malformation, these structures fail to separate completely, resulting in a single common channel for the passage of urine, stool, and reproductive fluids. This condition occurs in approximately 1 in every 25,000 births, making it a complex and challenging disorder to manage.
The Need for Cloacal Malformation Surgery
Cloacal malformation requires surgical intervention to restore normal anatomical function and improve the overall quality of life for affected infants. The primary goals of cloacal malformation surgery are to separate the common channel into separate urinary, gastrointestinal, and reproductive tracts, reconstruct the affected organs, and ensure proper functioning of each system.
Surgical Techniques and Challenges
Cloacal malformation surgery is a highly specialized procedure that requires a multidisciplinary team of pediatric surgeons, urologists, gastroenterologists, and gynecologists. The specific surgical approach depends on the severity of the malformation and the individual needs of the patient. The procedure generally involves an incision in the lower abdomen to access the common channel and the affected organs.
During the surgery, the surgeons meticulously separate the fused structures, creating separate pathways for urine, stool, and reproductive fluids. The bladder, rectum, and vagina are reconstructed using healthy tissues and muscles. In some cases, additional procedures may be required to address associated complications such as kidney abnormalities or spinal defects.
One of the significant challenges in cloacal malformation surgery is preserving and restoring normal bowel, urinary, and sexual function. Due to the complex nature of the malformation, the procedure carries a risk of postoperative complications, including urinary and fecal incontinence, urinary tract infections, and sexual dysfunction. Close monitoring and long-term follow-up care are crucial to address these challenges and provide necessary support to the patient and their family.
Potential Outcomes and Postoperative Care
The success of cloacal malformation surgery greatly depends on the severity of the malformation and the expertise of the surgical team. While each case is unique, the surgery aims to improve the child's ability to control urine and bowel movements, promote normal sexual development, and prevent long-term complications.
Following the surgery, infants require comprehensive postoperative care, including close monitoring of urinary and bowel function, management of wound healing, and ongoing evaluations of organ development. Physical therapy, behavioral support, and psychological counseling may be necessary to aid in the child's recovery and adjustment to normal daily activities.
Conclusion
Cloacal malformation surgery plays a vital role in addressing the complex anatomical and functional challenges faced by infants born with this rare congenital anomaly. Through specialized surgical techniques, a multidisciplinary approach, and comprehensive postoperative care, the surgical team aims to restore normal organ function and improve the overall quality of life for affected infants. Ongoing research and advancements in pediatric surgery continue to enhance outcomes and provide hope for a better future for these patients and their families.
We are associated with experienced and highly skilled medical professionals. We use the latest medical technology available in the world and we provide medical services in collaboration with JCI & NABH Certified hospitals only. Our services include various types of treatment and organ restructuring and transplant.
